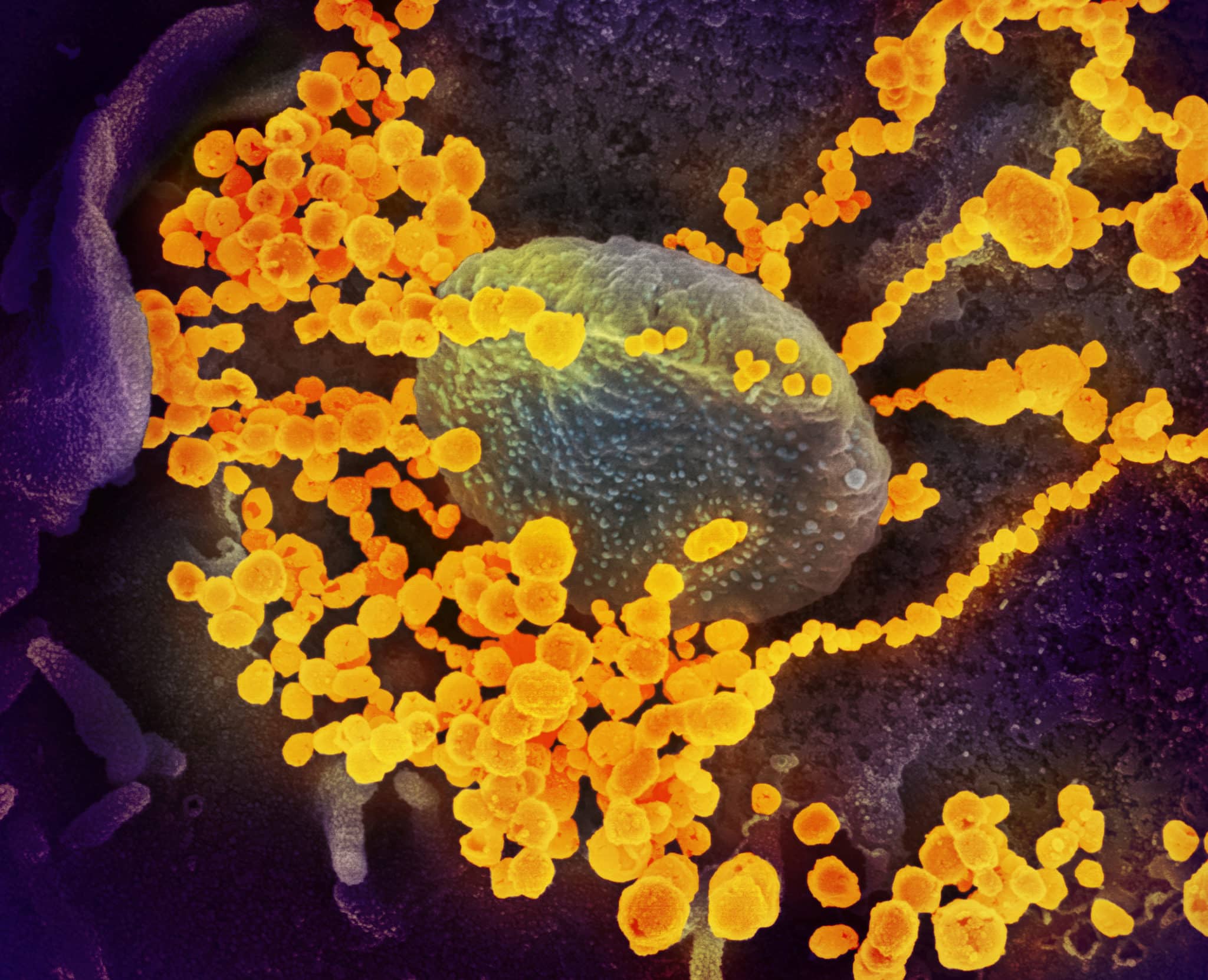
Scientists are only starting to grasp the vast array of health problems caused by the novel coronavirus, some of which may have lingering effects on patients and health systems for years to come, according to doctors and infectious disease experts.
Besides the respiratory issues that leave patients gasping for breath, the virus that causes COVID-19 attacks many organ systems, in some cases causing catastrophic damage.
“We thought this was only a respiratory virus. Turns out, it goes after the pancreas. It goes after the heart. It goes after the liver, the brain, the kidney and other organs. We didn’t appreciate that in the beginning,” said Dr. Eric Topol, a cardiologist and director of the Scripps Research Translational Institute in La Jolla, California.
In addition to respiratory distress, patients with COVID-19 can experience blood clotting disorders that can lead to strokes, and extreme inflammation that attacks multiple organ systems. The virus can also cause neurological complications that range from headache, dizziness and loss of taste or smell to seizures and confusion.
And recovery can be slow, incomplete and costly, with a huge impact on quality of life.
The broad and diverse manifestations of COVID-19 are somewhat unique, said Dr. Sadiya Khan, a cardiologist at Northwestern Medicine in Chicago.
With influenza, people with underlying heart conditions are also at higher risk of complications, Khan said. What is surprising about this virus is the extent of the complications occurring outside the lungs.
Kahn believes there will be a huge healthcare expenditure and burden for individuals who have survived COVID-19.
LENGTHY REHAB FOR MANY
Patients who were in the intensive care unit or on a ventilator for weeks will need to spend extensive time in rehab to regain mobility and strength.
“It can take up to seven days for every one day that you’re hospitalized to recover that type of strength,” Kahn said. “It’s harder the older you are, and you may never get back to the same level of function.”
While much of the focus has been on the minority of patients who experience severe disease, doctors increasingly are looking to the needs of patients who were not sick enough to require hospitalization, but are still suffering months after first becoming infected.
Studies are just getting underway to understand the long-term effects of infection, Jay Butler, deputy director of infectious diseases at the U.S. Centers for Disease Control and Prevention, told reporters in a telephone briefing on Thursday.
“We hear anecdotal reports of people who have persistent fatigue, shortness of breath,” Butler said. “How long that will last is hard to say.”
While coronavirus symptoms typically resolve in two or three weeks, an estimated 1 in 10 experience prolonged symptoms, Dr. Helen Salisbury of the University of Oxford wrote in the British Medical Journal on Tuesday.
Salisbury said many of her patients have normal chest X-rays and no sign of inflammation, but they are still not back to normal.
“If you previously ran 5k three times a week and now feel breathless after a single flight of stairs, or if you cough incessantly and are too exhausted to return to work, then the fear that you may never regain your previous health is very real,” she wrote.
Dr. Igor Koralnik, chief of neuro-infectious diseases at Northwestern Medicine, reviewed current scientific literature and found about half of patients hospitalized with COVID-19 had neurological complications, such as dizziness, decreased alertness, difficulty concentrating, disorders of smell and taste, seizures, strokes, weakness and muscle pain.
Koralnik, whose findings were published in the Annals of Neurology, has started an outpatient clinic for COVID-19 patients to study whether these neurological problems are temporary or permanent.
Kahn sees parallels with HIV, the virus that causes AIDS. Much of the early focus was on deaths.
“In recent years, we’ve been very focused on the cardiovascular complications of HIV survivorship,” Kahn said.
(Reporting by Julie Steenhuysen; additional reporting by Caroline Humer and Nancy Lapid in New York; Editing by Bill Berkrot)